It’s my life. What right do you have to tell me what I can do with it?
Voluntary euthanasia (VE) and physician-assisted suicide (PAS) are complex and touchy subjects. Both for the people who want to see them legalised and those who do not sincerely believe their views reflect the most humane option for the terminally ill. Let’s examine the arguments.
Many people, including those who advocate for voluntary euthanasia, are convinced that the personal autonomy of the individual is paramount. Surely, they argue, it is an individual’s right to decide how and when they die.
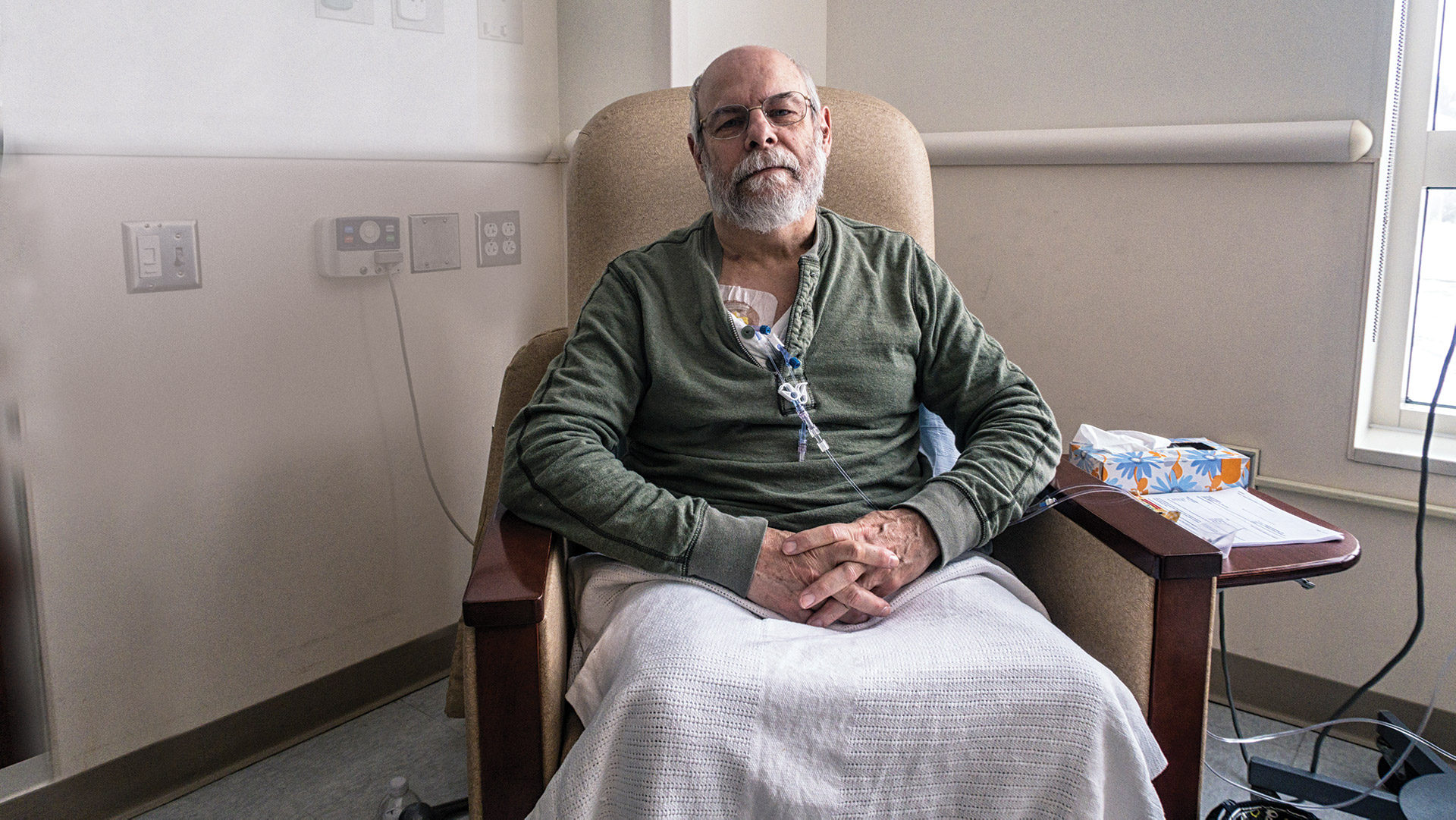
If a terminally ill patient wishes to die, should that patient really be forced against their will to continue a life they no longer wish to endure? It may seem self-evident that an individual has the right to determine their future. This includes the so-called “end of life choice” and it comes up whenever the whole issue is debated.
The right to be left alone
Is there a moral difference between killing someone and just letting them die? New Zealand’s Bill of Rights preserves citizens’ rights not to have medical treatment foisted upon them—they have the right to be left alone. Patients who sense the end of their lives approaching regularly request a “do not revive” note be added to their medical chart, and this is usually respected by hospital staff.
Moreover, the choice to end our lives is already permitted. For the past 127 years, suicide has not been a crime in New Zealand, although we are still not allowed to “aid and abet suicide” under the Crimes Act. In Australia, both assisted dying and physician-assisted suicide are illegal, except in Victoria. Australia generally regards decisions about both practices as matters for state governments or—in the case of the territories—the federal government. In short, while taking your own life is tragic and authorities will attempt to prevent you from harming yourself, you will not generally be prosecuted for attempting to do so.
It should also be noted that physicians are within the law when they take steps to relieve pain, even if they know this could have the incidental effect of hastening a patient’s death. For example, when an increased dose of morphine is given to a dying patient in a hospice, it often results in their dying earlier. But this practice is widespread and widely accepted, even by opponents of euthanasia. It is also lawful to withdraw life-preserving medical treatment when the ongoing treatment is, according to the best medical opinion, futile. Let us be clear that neither of these situations constitutes euthanasia.
Euthanasia and physician-assisted suicide refer to deliberate actions taken with the intention of ending a life.

MmeEmil—Getty Images
The limits to autonomy
Opponents of euthanasia argue that personal “autonomy” is not absolute. They point out that there are many other “autonomous decisions” that the government won’t have a bar of. We don’t have the legal right, for example, to decide to sell methamphetamines, to beat our spouse or not to wear seatbelts. So do we really have the right to ask others to help us take our own lives?
Healthy citizens may be told that the right to die belongs to those whose lives are no longer worth living—that is, in the opinion of a court, or a medical practitioner. So what starts out as an autonomous choice could, ironically, end up in the hands of others. It’s worth considering, too, that if VE were to be legalised, the elderly would be the group most at risk of being pressured into making a “voluntary” decision to end their lives.
Isn’t euthanasia basically compassionate?
An argument sometimes put forward in favour of “mercy killing” is that it is basically compassionate. If we put dogs and cats to sleep when they are suffering, why not our tortured, cancer-ridden mother? But this argument has its flaws also. It would perhaps be valid if we wanted to treat people the same way that we treat animals. But an analogy between animals and humans doesn’t really advance the cause of VE. Remember, it’s not just the loved family pets that we “put down” as a society, but also animals that are abandoned, unwanted, aggressive or simply a nuisance. Should we have the right to treat Grandma the same way?
In my view, the rise of palliative care and the hospice movement represents the genuinely compassionate approach to pain and suffering. Palliative care, as defined by the World Health Organization, “intends neither to hasten nor postpone death”. It is wholistic. Physical, emotional, spiritual, social and cultural needs are valued equally. Tellingly, Hospice New Zealand does not support voluntary euthanasia or assisted suicide in any form.
The view of the courts
Foundational to Western criminal law and to professional medical ethics is the principle that we cannot kill other people. Subject to exceptions like self-defence, human life is sacrosanct, even if the person in question has consented to it being terminated. The courts have consistently guarded the principle of the sanctity of life to protect the rights of the weak, the vulnerable and those with disabilities. They have recognised the distinction between letting a patient die and making that patient die.
Most medical associations worldwide have been firmly against the introduction of physician-assisted suicide. They say it would change the role of the doctor from healer to killer, and change it forever. The caring professional who has always saved lives would now become the one who took them. “Therapeutic killing” would inevitably erode patient trust.
Both voluntary euthanasia and physician-assisted suicide have been legalised in the Netherlands, Belgium, Luxembourg and Switzerland, as well as in four American states. That small number might suggest minority support for euthanasia, but a recent poll suggests 72 per cent of New Zealanders, including Prime Minister Jacinda Ardern, support some form of assisted dying. This month, New Zealand’s parliament will hold a national referendum on the issue. If the majority say they want it, a new law would allow terminally ill people with less than six months to live to choose assisted dying if this is approved by two doctors.

FatCamera—Getty Images
The slippery slope
There is some evidence from nations that have authorised VE that the availability of euthanasia expands to situations initially ruled out. In the Netherlands and Belgium, for example, euthanasia has been extended to enable minors to avail themselves of it (albeit with parental consent). Further, a small percentage of all deaths in the Netherlands and Belgium were cases of euthanasia implemented without the patient’s request (that is, involuntary euthanasia). A recent study found that 32 per cent of all physician-assisted deaths in the Flemish region of Belgium in 2007 were done without an explicit request from the patient. Nor has the requirement to report euthanasia always been complied with.
Some might argue that these outcomes could be avoided by building in legal safeguards so that a patient would have to consent to be euthanised. In practice, though, there would still be significant flaws. Terminally ill people are vulnerable to self-imposed pressure. They might come to feel that euthanasia would be “the right thing to do” because they don’t want to be a burden to their loved ones. Moreover, those who suffer from incurable illnesses might have families with a financial interest in their dying, and might be persuaded that they want to die or that they ought to want to die.
Summary
The arguments in favour of legalising VE and PAS may seem convincing. But on closer analysis, any VE law—even one carefully drafted with safeguards—is vulnerable to abuse. The frail elderly will inevitably feel euthanasia is the right thing to do to avoid “being a burden”. Finally, the legalisation of euthanasia would represent an irreversible alteration to the way society and the medical professional view the demise of the old and the terminally ill. Death would become planned and state-sanctioned in a way we have not seen before.
At stake is the meaning and value of human life.
Julie Belding is a freelance writer from Auckland. A more detailed treatment of the issues mentioned in this story can be found in the Killing Me Softly report published online at <familyfirst.org.nz>.
This article represents one side of the euthanasia debate. What’s your view? Join the conversation at <facebook.com/signsmag>.